Review Article
Year: 2022 |Volume: 3 | Issue: 03 |Pages: 27-32
Corneal Ectatic Disease - Progression
About Author
Correspondence Address:
Dr.Amit Chandankhede . Assistant Professor - Shalakya Tantra Department ,Shri Ayurved College Nagpur , PHD Scholar, Mahatma Gandhi Ayurved College , Hospital and research center, Salod (H), Wardha Email: dramitwc@gmail.com
Date of Acceptance: 2022-03-16
Date of Publication:2022-04-23
Article-ID:IJIM_154_04_22 http://ijim.co.in
Source of Support: Nil
Conflict of Interest: Nil
How To Cite This Article: Chandankhede . Corneal Ectatic Disease - Progression. Int J Ind Med 2022;3(3):27-32 http://doi.org/10.55552/IJIM.2022.3304
Abstract
: Before the appearance of recent tomographic imaging and membrane cross-linking (CXL), identification and treatment of ectatic unwellness was restricted to disease severity during which changes to the anterior corneal surface resulted in visual disturbances. Rigid contact lenses and/or penetrating corneal transplant treated advanced disease, as a result of early or subclinical identification of disease wasn't doable or its necessity was appreciated. The emergence of cardinal as a viable treatment to switch the natural progression of astigmatism has enlarged the requirement for higher diagnostics. Many strategies are delineated within the literature to assess and document the progression of keratoconus, however there's no consistent definition of the progression of ectasia. the foremost recent imaging techniques (eg tomography) have created it doable to notice ectatic unwellness early, before loss of vision and subjective disorders.Belin' ABCD classification/staging system was introduced on a Scheimpflug imaging system [Pentacam, (Oculus GmbH, Wetzlar, Germany)] to handle previous shortcomings. The ABCD system uses four parameters: anterior ("A") and posterior ("B" for the back) radius of curvature taken in an exceedingly three.0 metric linear unit optical zone targeted on the thinnest point, "C" is that the minimum membrane thickness and “D” vision of the most effective show distance. The primary 3 parameters (A, B, C) are mechanically generated objective measures that may be accustomed to confirm progressive change.The staging system isn't restricted to a selected industrial entity and might be incorporated in any tomographic imaging system. The ABCD Pro- gression show diagrammatically displays every parameter and shows once applied mathematics amendment on top of measuring noise is reached. this {could} permit the practician the power to diagnose progressive unwellness at a far earlier stage than was antecedently possible, with the arrogance that earlier intervention could stop visual loss.
Keywords: cross-linking, ectatic disease, keratoconus, progression, tomography.
Introduction
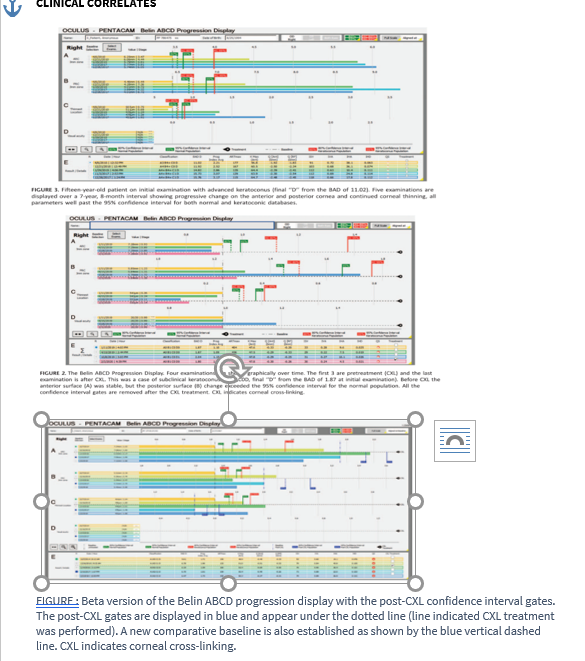
ABCD PROGRESSION DISPLAY :The Belin ABCD Progression show (Fig. 2) was designed to diagrammatically display the ABCD parameters over time with their associated 80% and 95% confidence intervals for each the traditional population information (broken inexperienced and solid green lines, respectively) and keratoconic population database (broken red and solid red lines, respectively).25,31,32. The baseline examinations are often marked and therefore the time of treatment indicated (eg, cross-linking) and shown by the black and white checkered line. As long as every examination meets internal quality checks, up to eight examinations over time will be displayed and are mechanically loaded by the Pentacam. Every parameter can then be examined over time and compared to the individual confidence intervals.31,32 Since CDVA is user-entered and not a machine-generated parameter, the “D” parameter doesn't think about intervals indicated., additionally, to the graphical show of the first ABCD parameters, ten supplementary tomographic/ topographic parameters are shown in tabular kind below the graphical display: [Belin-Ambrosio increased ectasis show (BAD) “D”, Progression Index Average (PIavg), Ambrosio relative Thickness most (ARTmax), Kmax, alphabetic character price 6.0 metric linear unit zone front, Q value 6.0 mm zone back, ISV, IVA, IHD, and therefore the ABCD classification].
The ABCD Progression show is meant to help the doctor and permit for earlier detection and documentation of progression. A recent study (Vinciguerra R. submitted for publication) found that quite half patients, already scheduled for cross-linking (based on >1 D change), might be known as progressive on the average five months earlier utilizing the fundamentals progression show.
Progression during this study was outlined as a minimum of a pair of the ABC parameters higher than the 80% confidence interval or one in all the ABC parameters above the 95% confidence intervals exploiting the additional rigorous astigmatism information (red gates on the display). The display may analyze historical knowledge and as such are often wont to review past records.
img
Discussion
POST CROSS-LINKING EVALUATION
Although unequivocal knowledge is missing on the precise turnover time of tissue layer albuminoid, corneal collagen undergoes a standard maturation and replacement, that raises the
question of cross-linking effective treatment duration. though progression determinants for astigmatism before 140 are established, less is thought concerning the post-CXL natural course, and tiny is known about post-CXL progression and also the potential want for repeat treatments. Currently, all the arrogance interval gates on the Belin ABCD progression show are removed once a 140 treatment is performed (Fig. 2). Post-CXL eyes, particularly those submitted to protocols with animal tissue removal (epi-off), bear a healing response which may embrace tomographic changes, epithelial remodelling, tissue layer thickness changes, and haze formation. 33,34 abundant of the healing response is assumed to be complete by the tip of the primary postoperative year, however the precise time of stabilization is unknown and certain extremely variable.35 to work out applicable progression parameters for post-CXL eyes, measuring noise once 140 had to be determined. In conjunction with the ELZA Institute (Zurich, Switzerland), the Ocular Cell Biology cluster at the University of Geneva (Geneva, Switzerland) and also the University of Arizona (Tucson, AZ), forty-one eyes of 41 patients (average age thirty-three years, vary 11–63) were enrolled. The average postoperative time since 140 was 13.5 months (range 9–23 months). All patients had a surgical diagnosis of astigmatism while not alternative comorbidities. lens system wear was interrupted a minimum of 1 week before measurements. 3 separate and consecutive Pentacam measurements were taken, removing the patient from the device between every measurement. A minimum of 7.5 millimeter of tissue layer coverage and an appropriate Pentacam quality score was needed for inclusion. Each pooled variance estimate and 1-sided confidence interval were computed victimization SPSS version twenty-three and STATA thirteen applied mathematics software package (same analysis employed in current ABCD progression display). each 80% and 95% one-sided confidence intervals were determined (Table 4).
Post-CXL knowledge is going to be incorporated within the next iteration of the ABCD Progression show (Fig. 7), wherever 80% and 95% confidence intervals for post-CXL changes can be shown by blue gates. These gates will solely seem if a treatment (CXL) is marked and also the post-CXL gates will only appear for the examinations once the treatment date. Of note and concern, however, is that our initial measuring noise post-CXL is considerably on top of the pre-treatment values. This might mirror incomplete healing, residual haze, or a testing amount that was too early post-CXL. We tend to presently evaluate patients a minimum of twenty four months post-CXL with further and bigger databases.
Conclusion
Multiple parameters and ways are planned to diagnose early ectatic illness and to outline progressive disease. Nevertheless, the worldwide accord on astigmatism and Ectatic Diseases (2015) declared that there's no consistent or clear definition of distention progression and acknowledged that specific quantitative information is lacking.7 during this sense, a lot of global assessment of the tissue layer would be more appropriate. The ABCD staging system incorporates anterior and posterior curvature, thinnest pachymetry values, and distance visual acuity. because it includes posterior curvature and thickness measurements supported the thinnest point, instead of top measurements, this staging system higher reflects the anatomical changes seen in astigmatism.25 Moreover, membrane thickness, anterior and posterior quantitative curvature values will function appropriate determinants for keratoconus progression.30–32 The capability for early identification and determinative progression at an earlier stage ought to give therapeutic intervention at an earlier stage, rather than later intervention with the potential for irreversible vision loss.
References
Nottingham J. Practical Observations on Conical Cornea: and on the Short Sight, and Other Defects of Vision Connected with it. London: J Churchill; 1854.
2. Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319.
3. Krachmer JH, Feder RS, Belin MW. Keratoconus and related non- inflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28:293–322.
4. Castro-Luna G, Pe ?rez-Rueda A. A predictive model for early diagnosis of keratoconus. BMC Ophthalmol. 2020;20:263.
5. Torres-Netto EA, Al-Otaibi WM, Hafezi NL, et al. Prevalence of keratoconus in paediatric patients in Riyadh, Saudi Arabi. Br J Ophthalmol.2018;102:1436–1441.
6. Amsler M. Kératocône classique et kératocône fruste; arguments unitaires. Ophtalmologica. 1946;111:96–101.
7. Gomes JA, Tan D, Rapuano CJ, et al. Global consensus on keratoconus and ectatic disease. Cornea. 2015;34:359–369.
8. Wittig-silva C, Chan E, Islam FM, et al. A randomized, controlled trial of corneal collagen cross-linking in progressive keratoconus: three-year results. Ophthalmology. 2014;121:812–821.
9. O’Brart DPS, Chan E, Samaras K, et al. A randomized, prospective to investigate the efficacy of riboflavin/ultraviolet A (370 nm) corneal collagen crosslinking to halt progression of keratoconus. Br J Ophthalmol.
2011;95:1519–1524.
10. Sykakis E, Karim R, Evans JR, et al. Corneal collagen cross-linking for treating keratoconus. Cochrane Database Syst Rev. 2015;3:CD010621.
11. Barbara R, Castillo JH, Hanna R, et al. Keratoconus expert Meeting, London, 2014. J Kerat Ect Cor Dis. 2014;3:141–158.
12. Mahmoud AM, Nun ?ez MX, Blanco C, et al. Expanding the cone location and magnitude index to include corneal thickness and posterior surface information for the detection of keratoconus. Am J Ophthalmol. 2013;156:1102–1111.
13. De sanctis U, Loiacono C, Richiardi L, et al. Sensitivity and specificity of posterior corneal elevation measured by Pentacam in discriminating keratoconus/subclinical keratoconus. Ophthalmology. 2008;115:1534–1539.
14. Tomidokoro A, Oshika T, Amano S, et al. Changes in anterior and posterior corneal curvatures in keratoconus. Ophthalmology. 2000;107:1328–1332.
15. Lopes BT, Ramos IC, Faria-Correia F, et al. Correlation of topometric and tomographic indices with visual acuity in patients with keratoconus. J Kerat Ect Cor Dis. 2012;1:167–172.
16. Guber I, McAlinden C, Majo F, et al. Identifying more reliable parameters for the detection of change during the follow-up of mild to moderate keratoconus patients. Eye and Vis 4. 2017;24. https://doi.org/10.1186/s40662-017-0089-3.
17. Kanellopoulos AJ, Asimellis Asimellis G. Revisiting keratoconus diagnosis and progression classification based on evaluation of corneal asymmetry indices, derived from Scheimpflug imaging in keratoconic and suspect cases. Clin Ophthalmol. 2013;7:1539–1548.
18. Suzuki M, Amano S, Honda N, et al. Longitudinal changes in corneal irregular astigmatism and visual acuity in eyes with keratoconus. Jpn J Ophthalmol. 2007;51:265–269.
19. Sandali O, El sanharawi M, Temstet C, et al. Fourier-domain optical coherence tomography imaging in keratoconus: a corneal structural classification. Ophthalmology. 2013;120:2403–2412.
20. Chatzis N, Hafezi F. Progression of keratoconus and efficacy of pediatric corneal collagen cross-linking in children and adolescents. J Refract Surg. 2012;28:753–758.
21. Choi JA, Kim MS. Progression of keratoconus by longitudinal assessment with corneal topography. Invest Ophthalmol Vis Sci. 2012;53:927–935.
22. Sorkin N, Varssano D. Corneal collagen crosslinking: a systematic review.Ophthalmologica. 2014;232:10–27.
23. Meiri Z, Keren S, Rosenblatt A, et al. Efficacy of corneal collagen cross-linking for the treatment of keratoconus: a systematic review and meta-analysis. Cornea. 2016;35:417–428.
24. Sklar JC, Wendel C, Zhang C, et al. Did collagen cross-linking reduce the requirement for corneal transplantation in keratoconus? The Canadian Experience. Cornea. 2019;38:1390–1394.
25. Belin MW, Duncan JK, Keratoconus. The ABCD Grading System. Klin Monbl Augenheilkd. 2016;233:701–707.
26. Ambrosio R, Belin MW. Imaging of the cornea: topography vs tomography. J Refract Surg. 2010;26:847–849.
27. Belin MW, Villavicencio OF, Ambrosio Jr . Tomographic parameters for the detection of keratoconus: suggestions for screening and treatment parameters. Eye Contact Lens. 2014;40(6):326–330.
28 Kanellopoulos AJ, Asimellis G. OCT corneal epithelial topographic asymmetry as a sensitive diagnostic tool for early and advancing keratoconus. Clin Ophthalmol. 2014;8:2277–2287.
29. Khachikian SS, Belin MW. Posterior elevation in keratoconus. Ophthalmology. 2009;116:816.
30. Duncan JK, Belin MW, Borgstrom M. Assessing progression of keratoconus: novel tomographic determinants. Eye Vis (Lond). 2016;3:6.
31. Belin MW, Meyer JJ, Duncan JK, et al. Assessing progression of keratoconus & crosslinking efficacy: The Belin ABCD Progression Display.Int J Kerat Ect Cor Dis. 2017;6:1–10.
32. Belin MW, Duncan J, Ambrosio Jr , et al. A new tomographic method of staging /classifying keratoconus: The ABCD Grading System. Int J Keratoconus Ectatic Dis. 2015;4:85–93.
33. Belin MW, Lim L, Rajpal RK, et al. Corneal cross-linking: current USA status—Corneal Society Guidance Document. Cornea. 2018;37:1218–1225.
34. Grisevic S, Gilevska F, Biscevic A, et al. Keratoconus progression classification one year after performed crosslinking method based on ABCD Keratoconus Grading System. Acta Inform Med. 2020;28:18–23.
35. Imbornoni LM, McGhee CNJ, Belin MW. Evolution of keratoconus: from diagnosis to therapeutics. Klin Monbl Augenheilkd. 2018;235(6):680–688.

